The PEPPER project brings together computer scientists, clinicians and industry leaders to create a personalised decision support system for diabetes management.
Diabetes is a widespread health condition that lasts for life. According to the World Health Organisation, there are about 60 million people with diabetes in the European Region. Type 1 diabetes often appears in childhood, but it can also occur in adults.

People with Type 1 diabetes traditionally manage their condition by drawing blood from their fingertips several times a day to test their blood sugar levels in order to calculate a dose of insulin to inject. If the dose is too large it can be fatal.

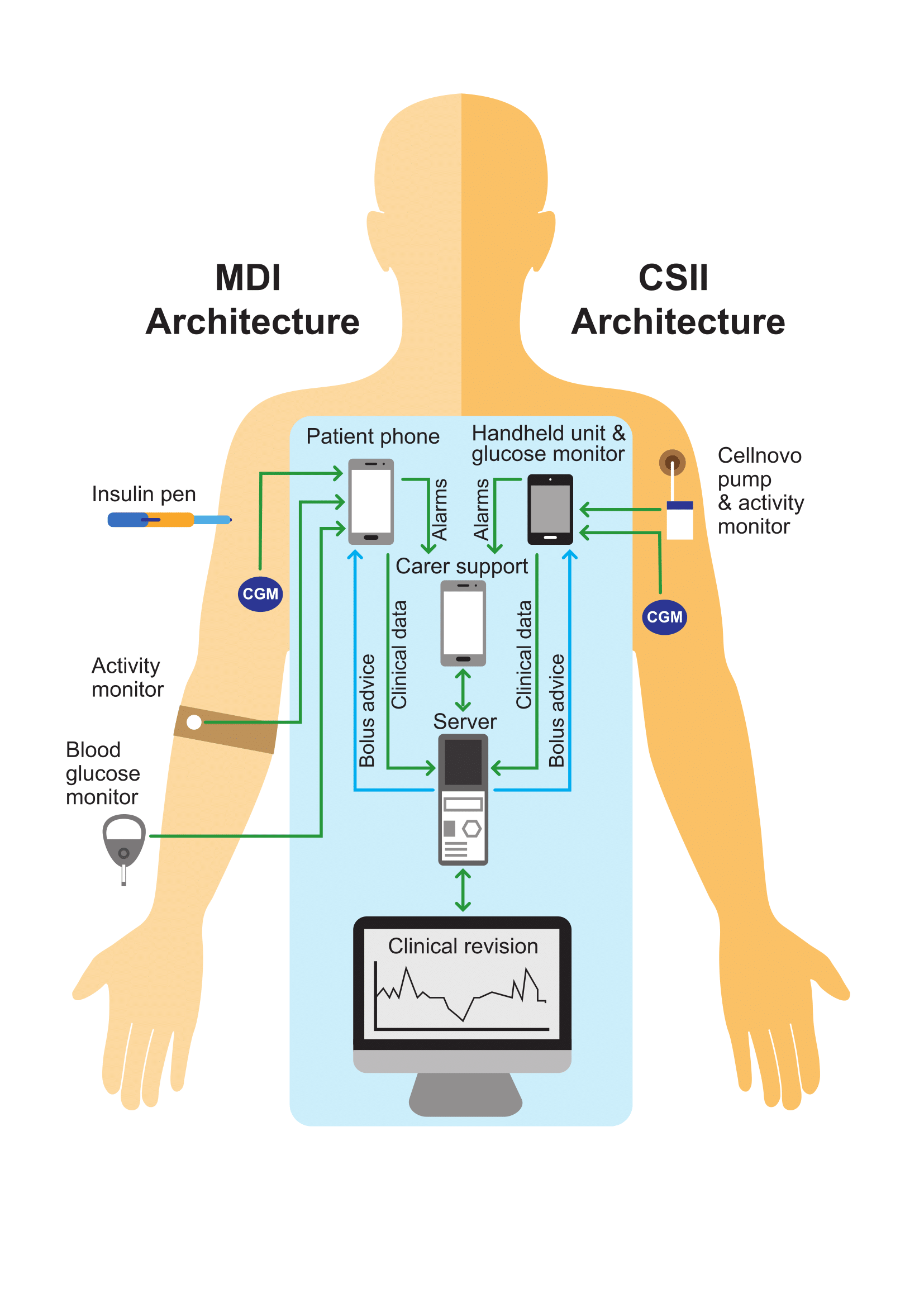
The advent of wearable technology offers hope both to adults and parents of young children with the condition. A growing number of people now administer their insulin via a wearable pump, and many also wear continuous glucose monitors. The PEPPER project is utilising such technology, together with artificial intelligence, to give people freedom from daily decision-making.
The PEPPER team is developing a personalised decision support system using case-based reasoning combined with predictive computer modelling. The system will make predictions based on real-time data in order to empower individuals to particiapte in the self-management of their condition. The design involves users at every stage to ensure that the system meets patient needs and raises clinical outcomes by preventing adverse episodes and improving lifestyle, monitoring and boosting quality of life. The project is also examining the extent to which human behavioural factors and usability issues have previously hindered the wider adoption of such personal guidance systems. It is being developed and validated initially for people with diabetes on basal-bolus insulin therapy, but the underlying approach can be adapted to other chronic diseases.

There is a strong emphasis on safety, with glucose predictions, dose advice, alarms, limits and uncertainties communicated clearly to raise individual awareness of the risk of adverse events such as hypoglycaemia or hyperglycaemia. The outputs of this research will be validated in an ambulatory settings and a key aspect will be innovation management. All components will adhere to medical device standards in order to meet regualtory requirements and ensure interoperability, both with existing personal health systems and commercial products. The resulting architecture will improve interactions with healthcare professionals and provide a generic framework for providing adaptive mobile decision support, with innovation capacity to be thereby increasing the impact of the project.

The project runs from 1 February 2016 until 31 January 2019 and includes the following partners: Imperial College London, Universty de Girona, Girona Biomedical Research Institute, RomSoft SRL and Cellnovo Ltd.
This project has received funding from the European Union's Horizon 2020 research and innovation programme under grant agreement No 689810.